Experience greater accessibility throughout the claims process
At Gallagher Bassett, delivering exceptional service to our customers has always been central to our mission. We continuously challenge ourselves to find better ways to swiftly resolve claims and achieve the best outcomes for everyone involved.
Whether providing clients with instant access to incident reports or connecting claimants with Resolution Managers, GBGO® mygbclaim has taken accessibility in the claims management process to the next level.
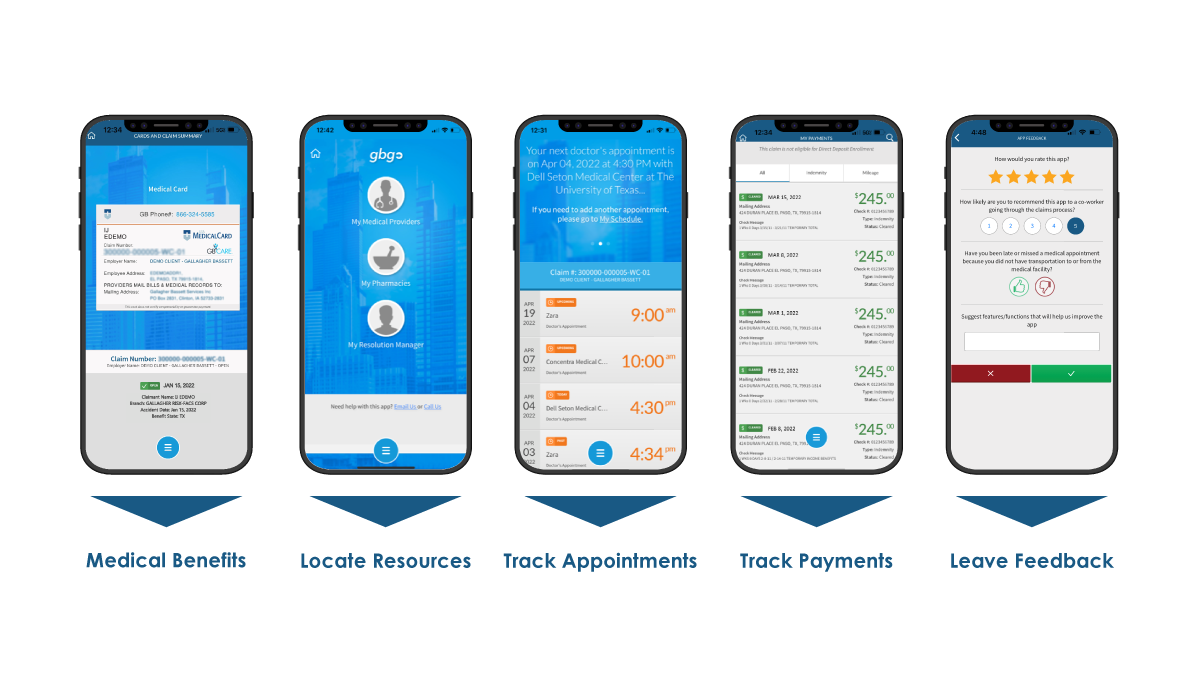
Important information at injured workers' fingertips
- Direct deposit
- Sign up for direct deposit of workers' compensation indemnity benefits (lost wages) through the app.
- Payments
- View benefit payments history and get notifications related to payment updates.
- Doctor's appointments
- Input the next doctor's appointment and let the app track it and send reminders.
- Claims FAQs
- Access answers to FAQs 24/7.
- Provider and pharmacy search
- Find a preferred medical provider or pharmacy nearby.
- Medical cards
- Access digital versions of the medical card and the pharmacy card (Rx card) with one click.
- Claims Resolution Manager communications
- Call or email the assigned claims representative with one click and send attachments (e.g., doctor's notes) via the app.
- Additional claims contacts
- Add, manage, and access claim contacts (e.g., RMs, providers, pharmacies) from one screen. Call or get directions to the provider location with one click.






